Chagas disease or American trypanosomiasis is a parasitic disease very common in rural areas of 21 Latin American countries (endemic countries). In recent years, due to the mobility of the Latin American population to other countries in the world, it has appeared in the USA and Europe, with Spain being the second non-endemic country with the highest number of cases. Roughly between 6 and 7 million people worldwide are infected. Between 50,000 and 90,000 infected people live in Spain, many of whom do not know they are ill. It is a chronic, silent, potentially fatal disease that can cause cardiac, digestive, and neurological diseases.
Causes and Transmission

In a natural environment, the reservoir is domestic animals (dogs, goats, cattle, pigs, horses, etc.) and wild animals, especially rodents and marsupials, as well as humans. The exception is birds, which are resistant to infection. Humans can acquire the infection by several mechanisms (vector bites, vertical or transplacental mechanism, blood transfusions, and blood products, organ transplants, and orally). The basic and main mechanism is by the bite of hematophagous triatomine insects of the genus Triatoma, Rhodnius, and Panstrongylus (“kissing bugs”), most of which are more active at night. When the triatomine bugs bite, they emit their droppings containing trypomastigotes, and when humans scratch the bite area, they drag the trypomastigotes along with them, allowing the parasite to penetrate through the bite area. In endemic areas, up to 50% of the triatomines are infected. Another common mechanism of transmission is vertical, from a pregnant woman with Chagas disease to the fetus, which can also occur in successive pregnancies (5-10 % transmissibility).
Outbreaks of American trypanosomiasis caused by ingestion of fruit juice or sugar cane juice contaminated with triatomine feces have been reported in highly endemic areas with large numbers of triatomine insects, such as Brazil and Colombia. Less frequently, the transmission of the protozoan occurs following blood transfusion or blood products, use of contaminated needles and syringes, or organ and tissue transplants.
Symptoms of American Trypanosomiasis
American trypanosomiasis has a first acute phase, which can be completely asymptomatic or present very mild symptoms, such as a slight fever, a feeling of general malaise, or inflammation of the area where the insect bite has occurred. And this is the problem with this parasitic infection since the affected person may not be aware that he or she is ill and may not go to the doctor for treatment. The symptoms, if they occur at all, remit without treatment, and the patient may remain asymptomatic for many years until the disease reactivates and enters a chronic phase with more severe symptoms:
- Constipation and other digestive disorders
- Malnutrition
- Abdominal pain
- Swallowing difficulties
- Hepatomegaly and splenomegaly (thickening of the liver and spleen)
- Heart failure
- Palpitations and heart rhythm disturbances that may cause heart failure
Approximately 30% of infected persons who are not treated in the acute phase of American trypanosomiasis will develop the chronic phase, although it may take up to 20 years from the time of the bite before the first digestive and cardiac problems occur. Once clinical heart failure has been reached, the patient dies within a few years. Heart rhythm disturbances (arrhythmias and tachycardias) can lead to sudden death.
Diagnosis
Various methods are available for the diagnosis of American trypanosomiasis. Currently, for the diagnosis of patients, the World Health Organization (WHO) recommends the performance of two tests based on different principles text antigens, and a third in case of discordance.
In general, the methods are classified as direct or indirect. Direct methods detect the parasite in the patient’s blood, usually called parasitological methods, and most are based on microscopy. There are also other techniques within this category, such as culture and xenodiagnosis (the latter based on the application of live insects directly to the skin of patients), whose use is very limited due to the high risk of infection of health personnel, the discomfort of patients or their impracticality. Indirect methods detect parasite DNA (molecular methods, especially polymerase chain reaction [PCR]) or anti-Trypanosoma cruzi antibodies in the patient’s blood (serological methods).
Treatment
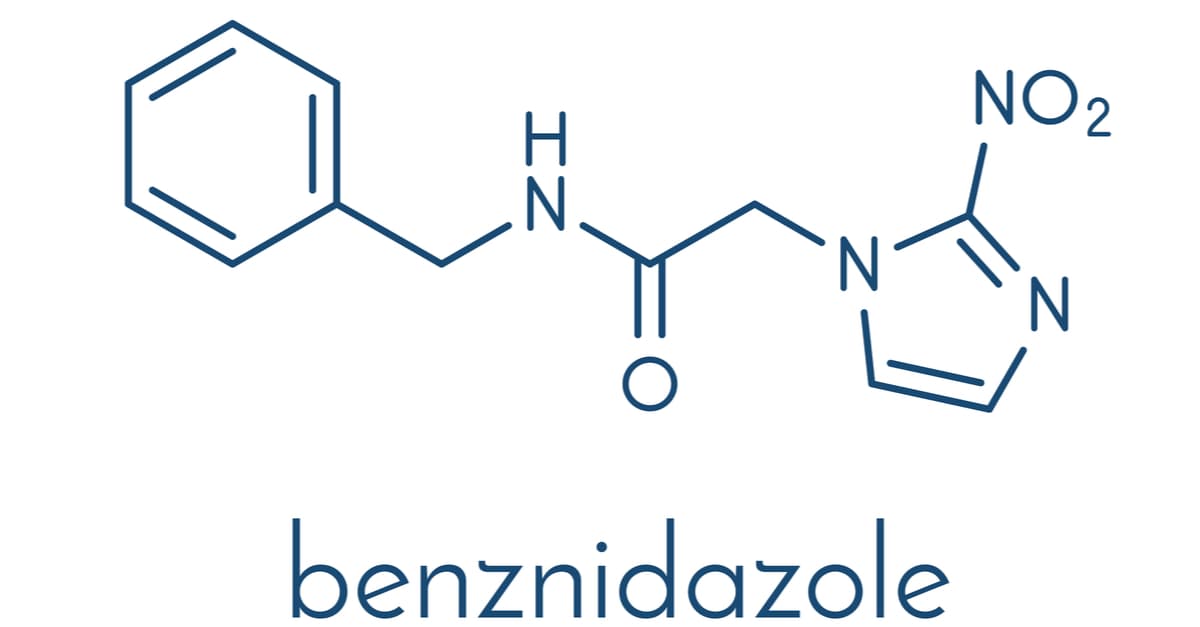
Treatment has two main objectives: Primary: to eliminate the parasite and contribute to reducing the probability of developing the clinical manifestations of the disease and its complications. Secondary: To contribute to the interruption of the T. cruzi transmission chain. The drugs used for treatment are Benznidazole and Nifurtimox. Benznidazole is considered the first choice therapy for the treatment of patients with American trypanosomiasis. Recommended doses of the drugs: Benznidazole: 5 to 10 mg/kg/day divided into two daily intakes, to be taken after food for 60 days, not to exceed the maximum daily dose of 300 mg. Nifurtimox: 10 to 15 mg/kg/day in children under 40 kg and 8 mg/kg/day in adults or over 40 kg. It is administered in 3 daily intakes, preferably after meals, for 60 days, without exceeding the maximum daily dose of 700 mg.

