Causes of Psoriasis
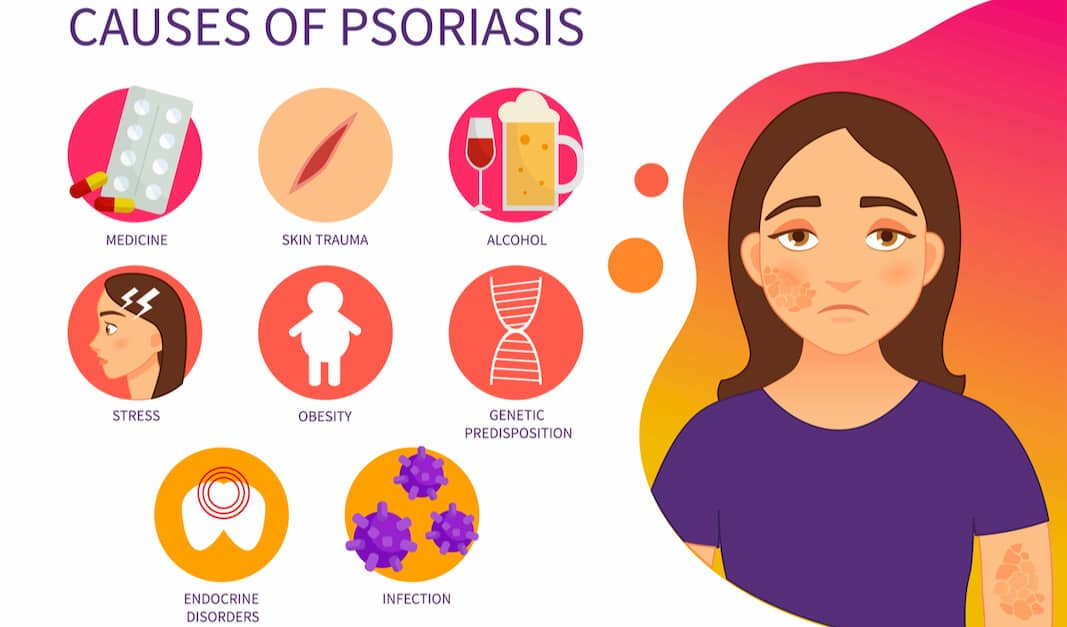
Even though the exact causes are not yet known, it is known that psoriasis is an autoimmune inflammatory disease, which has its origin in a disorder of the immune system. In the case of psoriasis, the immune system disorder causes the cells of the last layer of the skin, the keratinocytes, to grow much faster than usual: every 3-4 days instead of every 28 days, as occurs with cells from a person without psoriasis, giving rise to psoriatic plaques. Psoriasis occurs due to a combination of environmental and genetic factors. This means that it develops in a person likely to experience the condition because of the genes they received from their parents. However, a trigger is needed to set the whole process in motion. The primary triggers for psoriasis flare-ups are:
- Stress: Very frequent but can easily be controlled by the patient himself.
- Trauma: A direct blow to the skin can trigger psoriasis lesions in the affected area. This effect is known as the Koebner phenomenon and appears in 1 out of 4 patients. Other types of trauma, such as sunburn, postoperative scars, or drug eruptions, can also lead to psoriasis lesions.
- Bacterial or Viral Infections: can induce or worsen psoriasis lesions by activating the immune system’s cells.
- Medications: Some medications can contribute to flare-ups. That is why it is essential to inform the doctor of all the medicines the patient is taking.
- Climate: Cold and seasonal changes can cause psoriasis outbreaks.
- Other Factors: Alcohol, tobacco, and obesity have been closely linked to psoriasis flare-ups.
Symptoms

Psoriasis can come on gradually or come on suddenly. Also, symptoms may clear up over a period of time and reappear at another time. The most common symptoms are skin lesions in the form of plaques whose size can vary and which are characterized by being red and covered by whitish scales of different shapes and sizes. Some may be the size of the nail of the little finger. Still, others may extend to cover large surfaces of the body, adopting a ring or spiral shape. Desquamation can be confused with severe dandruff, but the characteristic plaques of psoriasis, which mix scaly areas with normal ones, distinguish it from dandruff. The eyebrows, armpits, belly button, and groin can also be affected. Other less frequent symptoms are:
- Pain.
- Genital injuries in men.
- Changes in the nails ranging from color (shades between yellow and brown), the nail’s thickness, and detachment and separation of the skin.
- Dandruff.
Treatment

The treatment of psoriasis depends on each patient and the type of condition they have. Although we still have no cure for this condition, it can be fully controlled, and in some cases, the symptoms (inflammation, redness, scaling, and itching) do not reappear. The different treatments that are applied are:
Topical Substances: The starting treatment for most psoriatic patients is usually creams, lotions, cleansers, and ointments applied to the affected areas.
Phototherapy: In general, the sun is of great benefit for these types of patients. However some may need a specific boost with artificial ultraviolet light (UVB rays), or a combination of UVB rays and medications, called PUVA (psoralen in conjunction with exposure to ultraviolet UVA light), also known as photochemotherapy. The drug is taken orally or injected to enhance the effects of UVA.
Systemic Drugs and Medication: Usually oral, although injectables may also be required:
- Steroids: Among the most commonly prescribed medication for mild and moderate psoriasis. They are drugs that mimic the action of certain hormones that the body produces naturally.
- Calcipotriol: it is a synthetic form of vitamin D, which is used in the treatment of mild or moderate psoriasis. It does not work quickly, but in the long term, it is effective in controlling psoriasis. It is not recommended to apply to the face area, where it can irritate.
- Retinoids: Derivatives of Vitamin A. They are usually used in combination with steroids.
- Anthralin: It is effective in mild or moderate psoriasis and does not pose long-term side effects, but it can be an irritant to the skin.
- Salicylic Acid: Salicylic acid is used as a complementary treatment. It is used to eliminate the scales of psoriasis plaques and prepare the skin for the application of topical medications.
- Methotrexate: Methotrexate dramatically clears psoriasis.
- Oral Retinoids (Isotretinoin): They are effective in some psoriasis cases but work best in combination with other medications. They are safe to use in long-term treatment.
- Cyclosporine: Controls the immune system. It is used only if all other options have failed. It is effective and quick-acting, but it can cause hypertension and may damage kidney function.

