Meningitis is a usually infectious disease caused by viruses or bacteria that lead to infection and inflammation of the meninges – membranes that surround the brain and spinal cord. When only the meninges are infected, it is called meningitis. Sometimes the bacteria enter the bloodstream and spread, which is called meningococcal sepsis. It can also happen that both problems occur at the same time.
What Are The Meninges?
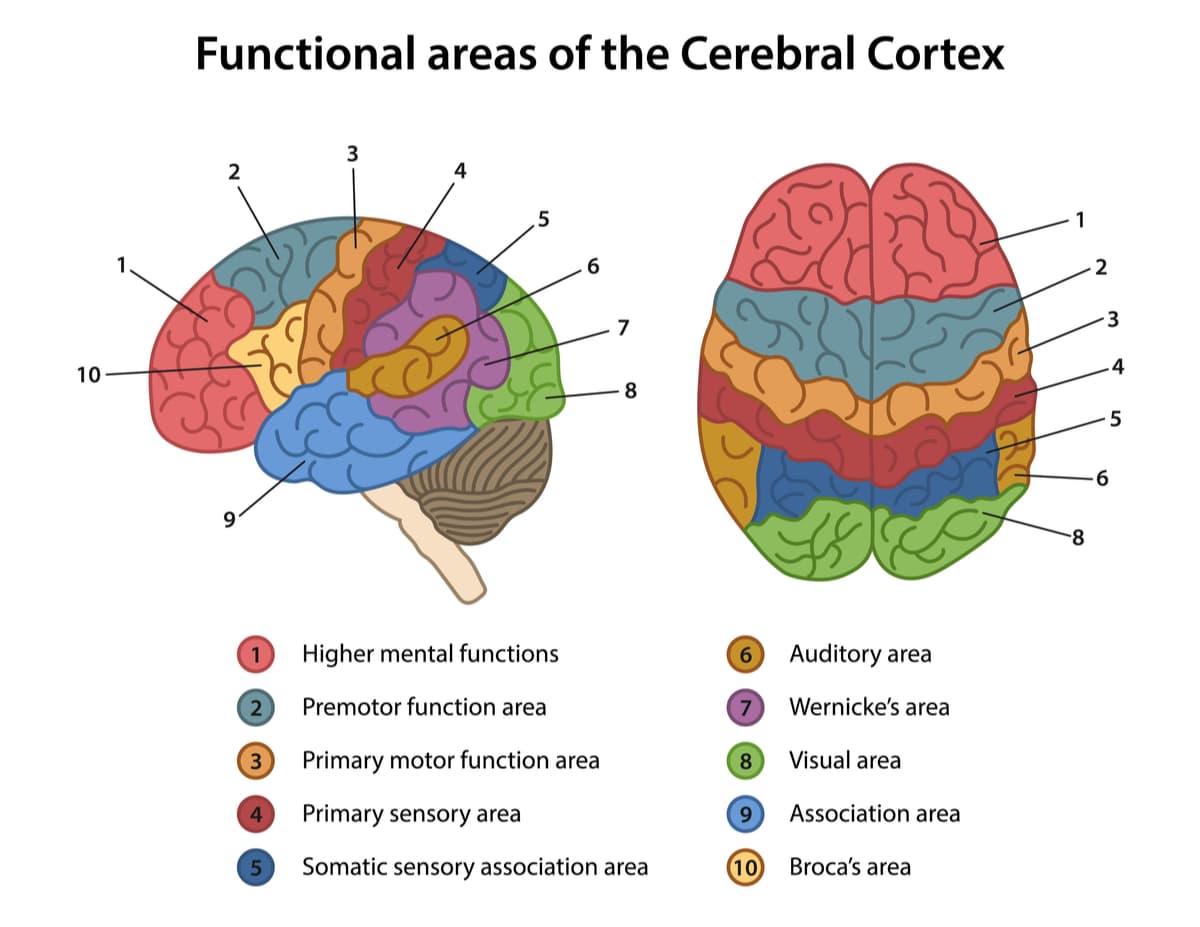
The meninges are three layers composed of specialized fibers and tissues, which are located above the cerebral cortex and in the spinal cord, with the main objective of providing a protection system that prevents the introduction of harmful substances into the brain and all the parts that compose it. These membranes can be located around the brain but also as an envelope of the spinal cord, i.e., they are structures that run around the outside of the central nervous system. In the case of the cerebral cortex, they are located below the skull.
Causes of Meningitis
Meningitis may be due to:
- Bacterial infections: These are a cause of severe meningitis. Many different microorganisms can be responsible for acute bacterial meningitis. The most frequent are bacteria called meningococci (especially in children and young people) and others called pneumococci (especially in adults). In addition to these bacteria, many others can also cause acute meningitis, such as streptococcus, Haemophilus, listeria, and other more infrequent germs. In general, the germs responsible for most of it come from our own nose or pharynx, from where, by mechanisms that are not well understood, they can infect the meninges. Sometimes, it occurs as a complication of an infection in a nearby site, such as otitis, sinusitis, mastoiditis, etc. In addition to acute meningitis, there may be bacterial meningitis with a slower course, such as tuberculous meningitis.
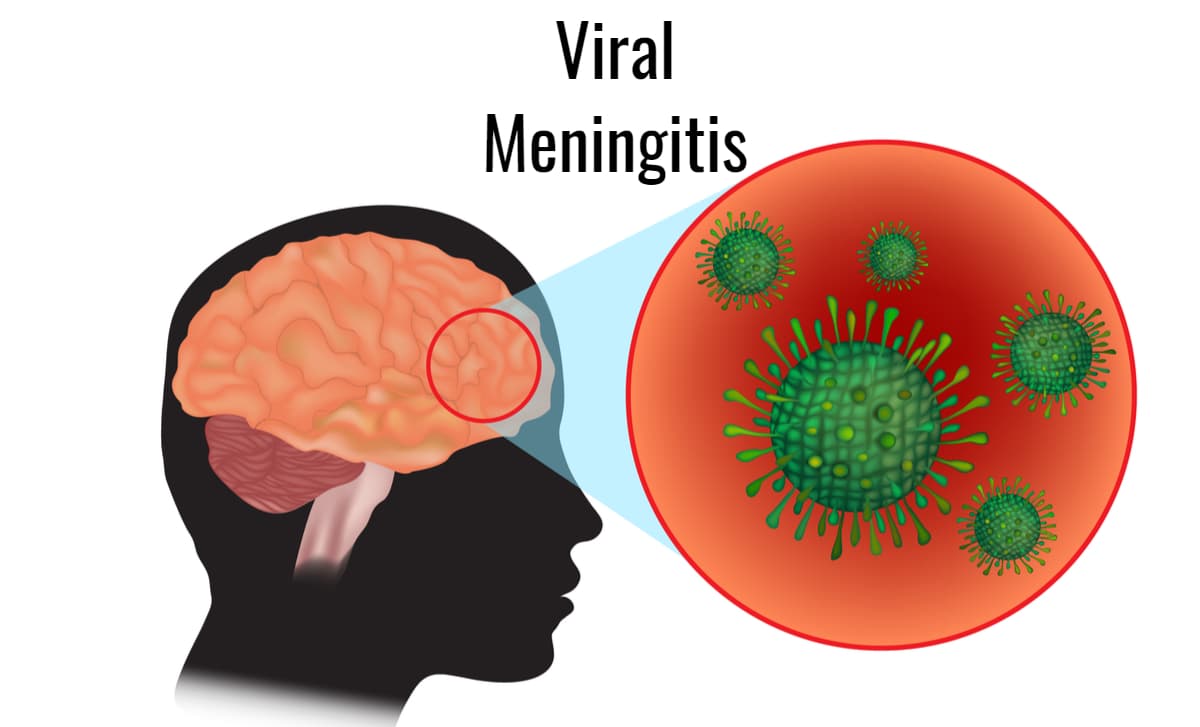
- Viral infections: Viral meningitis usually evolves benignly, without complications. Rarely, some viruses can produce serious and fatal infections, generally in people with low defenses.
- Fungi: These are rarer and occur mainly in immunosuppressed persons, such as persons receiving chemotherapy or immunosuppressive treatment.
Occasionally it may be caused by:
- Physical irritation (generally as a consequence of sunstroke).
- Chemical irritation (due to irritation of the meninges as a consequence of the introduction of some substance inside the subarachnoid space, such as contrast or medication).
- Infiltration of the meninges by cancer (carcinomatous meningitis).
Transmission of The Pathology
Transmission of this pathology occurs through saliva and droplets expelled when speaking, sneezing, or coughing. Transmission through objects is not common and occurs rarely. Meningitis usually occurs in the fall and spring. In settings such as daycare centers, schools, or nursing homes, it can spread rapidly. All forms of this illness are contagious. When a case of bacterial meningitis is detected, close contacts of the sick person (parents, siblings, caregivers, etc.) should see their physician for a specific course of antibiotics to prevent infection.
Symptoms
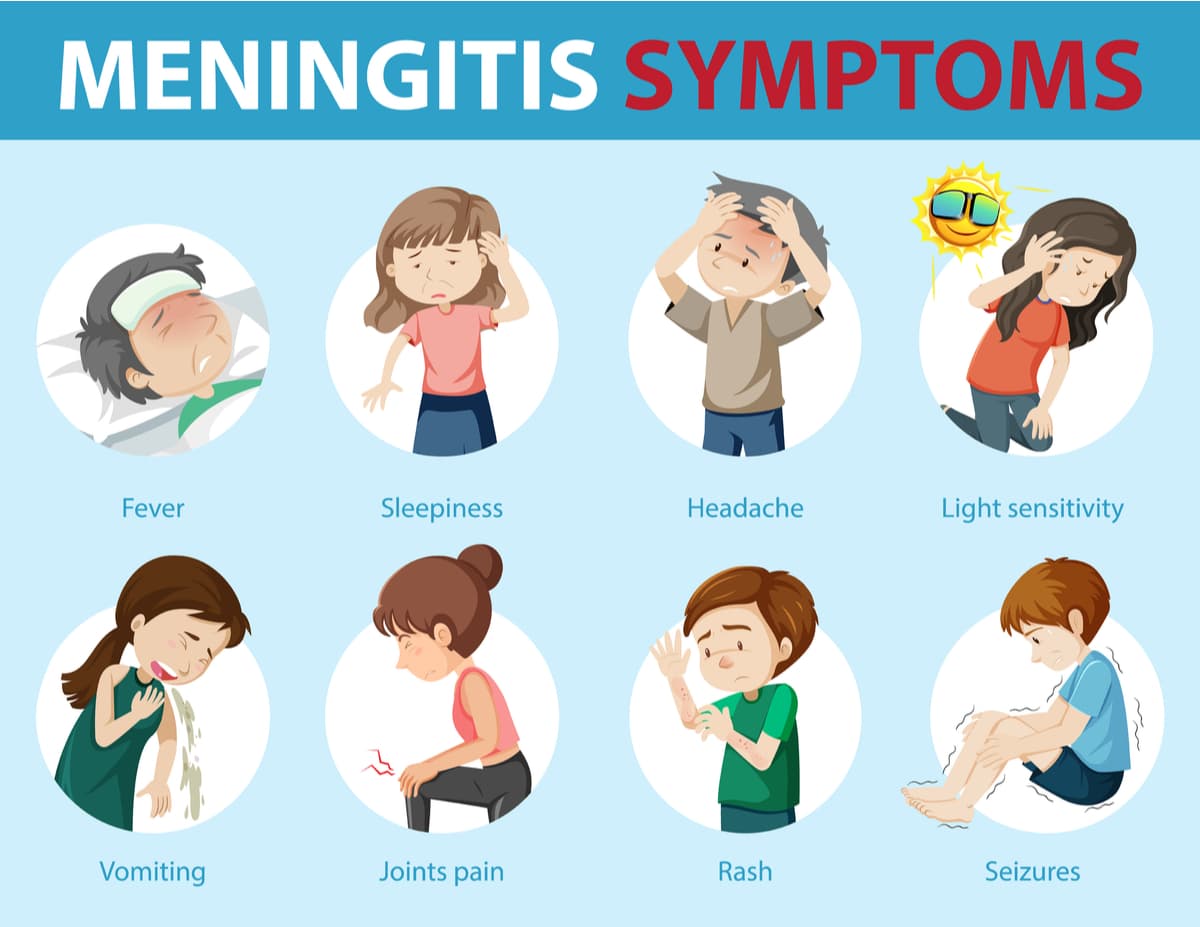
Meningitis is characterized by fever and headache. Because many diseases produce fever and headache, these symptoms are nonspecific. The headache, however, is usually more persistent than the headache associated with other infections and responds worse to treatment with analgesics. The rest of the symptoms may differ depending on the type.
Acute bacterial meningitis may progress:
- Over several days, starting with a catarrhal condition, fever and headache, followed by stiff neck, nausea, vomiting, decreased level of consciousness, drowsiness, neurological deficits (inability to move a part of the body, slurred speech, vision problems, etc.), seizures and coma.
- Fulminantly, within hours. This evolution is characteristic of some meningococcal meningitis. Reddish spots may appear all over the skin, which does not disappear when pressed and indicate a severe course of infection characterized by alterations in blood coagulation. If there is a fulminant course (Waterhouse-Friderichsen syndrome), the patient may go into shock, multiorgan failure, and coma, with a very high mortality rate only hours after the onset of symptoms.
Viral meningitis symptoms:
- This form usually progresses benignly in people with normal defenses, with fever, headache, eye pain, or discomfort with light, mild lightheadedness, and moderate neck stiffness. There may also be general malaise, muscle aches, loss of appetite, nausea, vomiting, abdominal pain, and diarrhea. In viral meningitis, there is no decreased level of consciousness, no neurological deficits, no seizures, and no coma, unless there is meningoencephalitis, i.e., an associated infection of the brain.
Treatment

In the case of acute bacterial meningitis, a delay in diagnosis and antibiotic treatment may result in permanent brain damage with severe sequelae and even death. For this reason, when acute bacterial meningitis is suspected, urgent intravenous antibiotic treatment should be started, even before performing the diagnostic lumbar puncture. At first, broad-spectrum antibiotics are used, and, later, when the results of the culture and antibiogram are available, the treatment is adjusted to the agent identified. With appropriate treatment administered in a timely manner, even patients with potentially severe meningitis can make a good recovery without sequelae.
Prevention

Usually, when a case of bacterial meningitis appears in a group, for example, at school, a short course of a specific antibiotic is administered to the people who have been in contact and who, therefore, may be pharyngeal carriers in order to prevent the disease from spreading. The best prevention is vaccination. Until recently, there were only vaccines against Haemophilus influenzae type b (Hib), meningococcus type A and C, and pneumococcus, which had practically eliminated these types of meningitis in our environment. Today there are vaccines against almost all types of bacterial meningitis.

